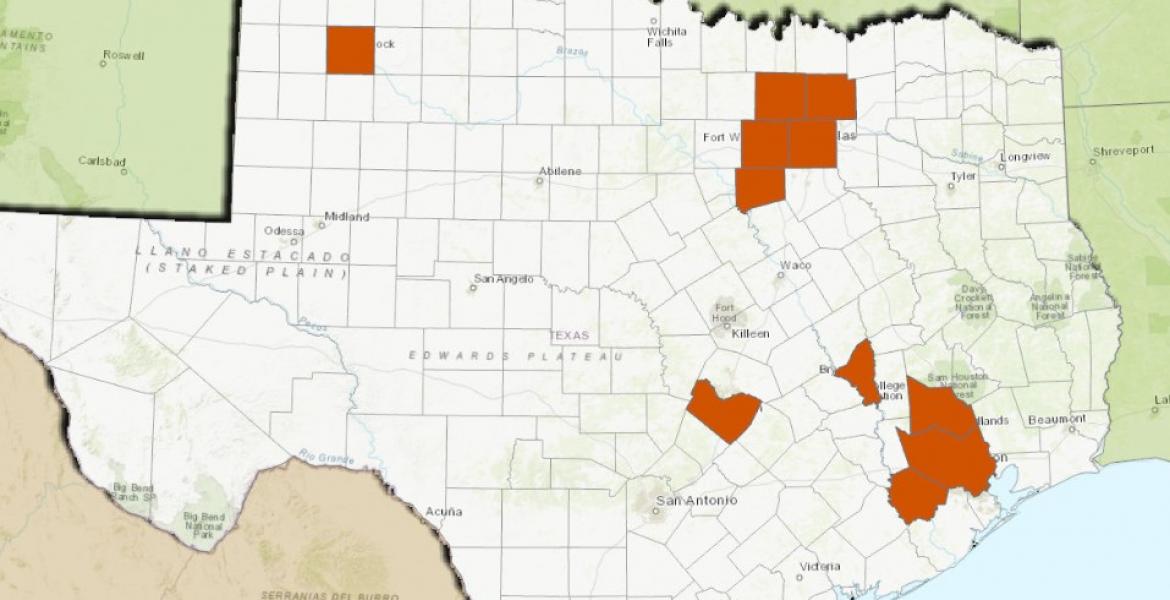
Nearly 50 people are being monitored for symptoms of the Ebola virus in Dallas after the death of Thomas Eric Duncan and the positive diagnosis of a Texas Health Presbyterian Hospital worker who provided care for him in the week and a half before his death.
The updated contact list was released by the Texas Department of State Health Services on Monday, which includes 10 contacts with definite exposure and 38 contacts with possible exposure as of 5 p.m. Sunday.
The list was initially released on Oct. 2, six days before Duncan, the first person to be diagnosed with the virus in the U.S., succumbed to the disease in Dallas. The list initially included roughly 100 individuals. Public health officials will attempt to reach all contacts and possible contact on a daily basis to check for fever and other symptoms, a news update states. The daily checkups will continue for 21 days after exposure.
The Dallas health care worker was not a part of the 48 contacts health officials are currently monitoring, and that list includes only individuals who might have had contact with Duncan prior to Sept. 28, which is the day he was admitted to Texas Health Presbyterian.
So far, only one person known to have close contact with the healthcare worker who treated Duncan is thought to be at risk for contracting the virus, however the Centers for Disease Control (CDC) is evaluating other potential exposures as well and working to compose an updated list of individuals for monitoring.
Texas health officials received preliminary positive test results for the health care worker from a lab in Austin at 9:30 p.m. on Saturday, and indicated in a press release that the level of her symptoms suggests that the level of the virus she has is low, a CDC press release states.
The worker, whose identity has been masked, developed symptoms on Friday last week and was immediately put into isolation, tested and monitored. How and when she contacted the virus is still unclear.
“We don’t know what occurred in the care of the index patient—the original patient in Dallas—but at some point there was a breach of protocol and that breach in protocol resulted in this infection,” CDC Director Tom Frieden said in a press briefing Sunday.
At this point, Frieden said, the CDC is doing four things to handle the situation, including, safely and effectively caring for the patient; assessing her possible contacts; evaluating other potential health care worker exposures; and conducting a complete investigation into how the infection occurred.
“…unfortunately, it is possible in the coming days that we will see additional cases of Ebola,” Frieden said. “This is because health care workers who cared for this individual may have had a breach of the same nature of the individual who appears now to have preliminary positive tests. That risk is in the 48 people who are being monitored, all of them have been tested daily, none of whom so far have developed symptoms or fever, and in any other health care workers who may have been exposed to this index patient while he was being cared for. We’re still determining how many health care workers that will be.”
Instructions for protocol and procedure when dealing with Ebola patients have been disseminated to hospitals nationwide, and a push to limit the number of health care professionals who have contact with infected patients are measures the CDC and hospitals are taking to prevent further transmission, Frieden said. Integral to fighting an outbreak is breaking transmission chains, he said.
“That’s how we have stopped every Ebola outbreak in history excep the one currently in West Africa,” he said. “That’s how we stopped it in Lagos, Nigeria. That’s how we will stop it in Dallas. So breaking the link in the chain of transmission is key to preventing further spread.”
Following the death of Eric Thomas Duncan on Oct. 8, the CDC announced plans to enhance Ebola screening at five U.S. airports that receive over 94 percent of travelers from Ebola-affected nations. Dallas/Fort Worth International Airport was not on that list.
Screening began at JFK International Airport on Saturday, and is anticipated to begin on Thursday at Washington-Dulles, Newark, Chicago-O’Hare and Atlanta International.
A press release from the CDC states that screening begun two months ago in three countries, and of the 36,000 screened, 77 were denied boarding a flight. None of those, however, were diagnosed with Ebola, and many were found to have malaria.
The release lists four steps that will be taken after passport review as part of the screening process:
- Travelers from Guinea, Liberia, and Sierra Leone will be escorted by CBP to an area of the airport set aside for screening.
- Trained CBP staff will observe them for signs of illness, ask them a series of health and exposure questions and provide health information for Ebola and reminders to monitor themselves for symptoms. Trained medical staff will take their temperature with a non-contact thermometer.
- If the travelers have fever, symptoms or the health questionnaire reveals possible Ebola exposure, they will be evaluated by a CDC quarantine station public health officer. The public health officer will again take a temperature reading and make a public health assessment. Travelers, who after this assessment, are determined to require further evaluation or monitoring will be referred to the appropriate public health authority.
- Travelers from these countries who have neither symptoms/fever nor a known history of exposure will receive health information for self-monitoring.
The Ebola virus is transmitted through contact with bodily fluids. Rumor of the virus mutating and becoming airborne has been discounted by the World Health Organization (WHO), who recently released a statement reading, "At this point in time we have no evidence and do not anticipate that the Ebola virus is mutating to become airborne."
For more information on the Ebola virus, visit the CDC or WHO website.
Subscribe to the LIVE! Daily
Required




Comments
Listed By: Debbie Cunningham
- Log in or register to post comments
PermalinkListed By: J D
- Log in or register to post comments
PermalinkPost a comment to this article here: