SAN ANGELO, TX – Today, a patient in his 60s, suffering from coronary artery disease, was the first to undergo a new treatment option that disappears over time at San Angelo Community Medical Center.
This patient is the first in the area to have the world’s first FDA-approved dissolving heart stent deployed into an artery.
Dr. Michael Blanc, an interventional cardiologist, Medical Director of the Heart and Vascular Center at SACMC, and who has spent 25 years researching and utilizing stent technology to help patients, said the man had suffered a heart attack a week ago.
The patient had a smaller artery that had a metal stent with the drug coating, but he had a much bigger blood vessel area that had a critical narrowing of it. Thus, Dr. Blanc and his team waited a week because they knew today was the day—the day for the Absorb bioresorbable heart stent, approved by the FDA on July 5, 2016, would become available to patients by only a handful of hospitals across the nation.
Community is one of these few hospitals, and Dr. Blanc, his team, and the Community Medical family were proud to lead this day using such groundbreaking technology.
For the patient, Dr. Blanc said it will be helpful for him to have this in that large artery. As for the procedure itself, it went good, and the patient is doing well, he said.
SACMC Chief Executive Officer Jeremy Riney said this new procedure helps to advance the hospital’s cardiac program, and he and his staff are always trying to find ways to do things better today than they did yesterday for the sake of their patients.
“First and foremost, it’s about the positive outcome for the patient, and that’s what we do every day here,” said Riney. “We have the patient first in mind, and technology, coupled with that focus, leads to a good accomplishment at the end of the day. That’s what’s most important for us.”
More About the New Dissolving Heart Stent
Dr. Blanc said this is the first new stent used on patients who suffer from coronary artery disease available in the last 12 years.
“It’s a stent that we’ve been waiting on for 20 years,” he said. “The whole concept that the stent will dissolve is [one] we wanted to have since we started placing stents in for the first time in 1993.”
This stent dates Blanc’s time at Community, being that he started this procedure in 1992 when stents were first available.
“So, I’ve actually seen the whole spectrum of things happen where we put stents in, and we had a high risk of arteries re-narrowing of about 1 in 3, until we put in drug coated stents in 2003, and that number went down to about 1 in 20,” he said.
Now, with this stent, re-narrowing risks are about the same, but Dr. Blanc said the nice thing about it is, within 18 to 24 months, the stent is completely absorbed out of the body. It works similar to dissolvable stitches and sutures.
“There’s no stent material left,” said Dr. Blanc. “The arteries are able to heal, but the stent goes away.”
Dr. Blanc noted that, as this technology evolves, and being on the second generation of stents, which has been refined over the last few years, implanted now for 10 years, and put in over 200,000 patients worldwide, the goal is to refine the second generation.
“There are over 80 or 100 other companies looking at new different kinds of stent materials that are bioresorbable,” said Dr. Blanc. “I think that is where the future growth of these stents are because, when God put us on this earth, he didn’t put stents inside our arteries. We’re there to help fix the artery, but then get it back to the kind of artery that dilates more normally, and works more normally.”
Bioresorbable refers to a type of material that can be broken down naturally and then “resorbed” by the body.
Previously the stent, used since 1993, has been a metal one consisting of stainless steel with some alloy; and the initial stents did not have a drug coating on them. In 2003, those stents came with a drug coating so the risk of re-narrowing of that artery was reduced, explained Dr. Blanc.
“These stents are not made out of any metal,” he continued. “They’re made out of a material called polylactic acid, which is like lactic acid that we produce when our muscles are working hard. It will find a way to have lactic acid formulation that can give us enough strength to hold the artery open, but then, in a matter of 18 to 24 months, when we would get rid of lactic acid in our body, the body absorbs the lactic acid and our arteries return back to normal.”
For those patients who have a metal stent, unfortunately it will remain so permanently. The stent is like rebar that goes on a highway, said Dr. Blanc. It gets a cement layer over it anywhere between four weeks and three months after a stent is put in, so those stents can’t be removed from the body.
“But if they get a new blockage, which unfortunately does happen in folks, we would, at that point, decide what kind of stent would be best available,” added Dr. Blanc. “That would either be the bioresorbable stent, or a metal stent with the drug coating.”
Either way, Dr. Blanc said worldwide extensive research on this stent shows that the two are equivalent in keeping the arteries open, and the bioresorbable stent also has a drug coating over it, so it heals normally.
There’s also low risk of narrowing of that blood vessel, and the blood vessel does dilate more normally. Parts of the blood vessels are preserved better with the bioresorbable stents, and if someone needs bypass surgery, that stent goes away. Cardiologists can sew a bypass graft into the area of vessels and stent it easily, Dr. Blanc stated.
With a metal stent, cardiologists cannot sew a bypass graft into that area easily, he added.
Check out more here.
The Benefits and How the Procedure Works
Dr. Blanc said the procedure for deploying this new stent is no different than the standard one his staff has been performing for the past 25 years.
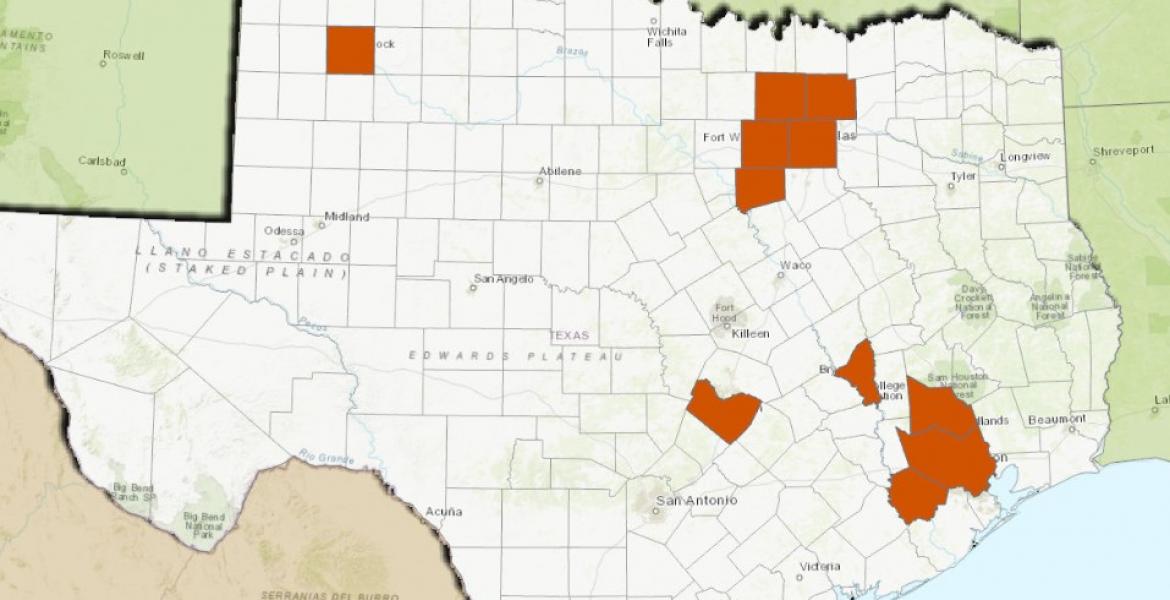
Being one of the few hospitals to offer this stent to patients is very exciting, said Dr. Blanc. Lubbock, Midland, and El Paso do not have this technology as of yet.
“I think the ability for us to provide this stent for patients just gives them another option as far as treatment,” he said.
Below: This video provides an in-depth look of the procedure (Video provided by SACMC and Abbott)
[[{"fid":"25187","view_mode":"default","type":"media","attributes":{"alt":"7826651 Video Absorb Mechanism of Action Animation narrated 0630","height":"562","width":"750","class":"media-element file-default"}}]]
Dr. Blanc explained that we were born with arteries that normally dilate to improve blood flow to the heart, and that’s one of the nice things about this stent. It will dissolve, so the artery has the ability to dilate more naturally.
“For a younger patient, if [he or she] must undergo future bypass surgery, the stent dissolves; and if a cardiologist has to sew a bypass into that artery, there’s a place for it to be sewn into the artery,” said Dr. Blanc.
Additionally, it’s a nice option if a cardiologist has to put multiple stents in an artery to “knock out having to put a lot of metal stents,” which the artery will not be able to absorb, and the body will not have for the blood vessel to dilate normally.
Dr. Blanc said he has a team in the “Cath Lab” (Cardiac Catheterization Laboratory) who works with him. There are several nurses, a Scrub Technician, a monitor technician and monitor assistant. There are multiple factors involved in putting in the stent.
“We don’t just do an X-Ray; we actually do an ultrasound from within the body inside the blood vessel so we can size the stent to make sure we’re putting the appropriate sized stent,” he explained. “Matching the stent size to the artery size is very important to this technique. It takes a little bit more technical expertise to put this stent in.”
Dr. Blanc said he feels that’s one of the reasons Community was able to get the stent there, because of the number of stent procedures he has performed.
“I’ve done over 5,000 interventions in my career, and I think they wanted to get this device into areas where people had a lot of experience,” he said.
The patients who benefit from this include anyone at risk for having artery blockage, and that can start at 25 up through the age of 85 to 90.
“It all depends where the blockage is, and the many characteristics of the blockage,” said Dr. Blanc.
However, Dr. Blanc noted middle-aged people will benefit more from this stent because they may have future blockages and need bypass surgery, so this gives more options to those patients.
As for wear and tear on the artery, Dr. Blanc said the arteries are amazingly resilient to doctors putting stents in them. They are a muscular structure, and the stent does very little damage to the artery.
Dr. Blanc concluded that the procedure is very similar to putting in the metal stents. The stents are just a little more rigid than the new ones. They are similar to the stents he put in 15 to 20 years ago.
“So there’s a few little technical things involved with preparing the blood vessel to make the stent go in,” he noted “That’s where having a few gray hairs, and a few cases behind you helps in determining how to get those stents in those patients.”
After Dr. Blanc fixes the arteries, however, the process doesn’t stop. Coronary disease is progressive, so even though doctors limit one area of critical blockage, it’s important for patients to keep their cholesterol down, walk for 30 minutes five days a week, and to do all things necessary to minimize future blockage.
What This Means for Patients Out of the Area
Dr. Blanc said there hasn’t been a big outpour of hospitals or doctors outside of San Angelo wanting to send patients to Community for the new stent, but the hospital does have a “great referral system” that will let other medical professionals know this is available to them.
“We’re more than willing to help any patient out who would want to have this as an option,” he said. “It’s not for every patient. Probably about 30 to 40 percent of patients who have blockages, this stent is appropriate. Another 60 percent, the older stent is completely appropriate for those patients.”
As for being on the cutting edge of medical technology, Riney said it’s always a great thing.
“Medical technology is advancing more and more every day,” he said. “New physicians coming out of training, we want to be able to have the latest technology available to them at their disposal. We want to provide that to our patients and our physicians. This instance is one where it provides a great clinical outcome for the patient and something that’s very satisfying for the physician as well.”
Other cardiologists at SACMC are interested and training to utilize the new stent, said Riney.
He said, “It’s always good to be the first, or at the top tier, on certain outcomes, and certain technology. But the fact that it’s going to produce a good clinical outcome for the patient is the most important thing.”
At an administrative level, this is something Community administrators and medical staff have been talking about for several months. They knew the technology was coming, and undergoing clinical trials. Dr. Blanc has spent a lot of time studying the data, and the medical team had to evaluate if it would be beneficial to the patients and the community they serve, said Riney.
“There’s a lot of time and effort that went into this,” he noted.
Thus, they “decided to pull the trigger on providing this technology, and it was about team work, getting people in the right places, getting the training in place for the staff and cardiologists, and making today happen,” Riney concluded.
Subscribe to the LIVE! Daily
Required




Post a comment to this article here: